What Is DOT Drug Testing and Why Compliance Matters
Managing a laboratory serving transportation clients means compliance demands far beyond standard workplace testing. Laboratory managers across the United States face unique challenges when handling DOT drug testing, where federal law prescribes every detail, from test panels to documentation. The Department of Transportation requires that each specimen you process aligns exactly with national standards—there is no room for shortcuts or missed steps. This overview explains what sets DOT protocols apart and how precise procedures protect your lab and clients.
Table of Contents
- Defining DOT Drug Testing for Laboratories
- DOT Drug Test Types and Testing Methods
- Key Regulations and 2026 Testing Updates
- Employer Roles and Laboratory Compliance Duties
- Risks, Penalties, and Avoiding Common Mistakes
Key Takeaways
| Point | Details |
|---|---|
| DOT Drug Testing Regulation | DOT drug testing is federally regulated and differs significantly from standard workplace testing, requiring strict adherence to procedures and documentation. |
| Mandatory Testing Scenarios | Testing must occur at specific employment stages such as pre-employment, post-accident, and random, each with unique requirements. |
| Role of Qualified Personnel | Collection and analysis must involve certified personnel, and results require review by a Medical Review Officer before reporting. |
| Compliance and Documentation | Accurate documentation and adherence to protocols are critical to avoid liabilities and ensure the integrity of test results. |
Defining DOT Drug Testing for Laboratories
DOT drug testing refers to a federally mandated substance screening program established under the Omnibus Transportation Employee Testing Act of 1991. For laboratory managers, understanding this distinction matters because DOT testing operates under a completely different regulatory framework than standard workplace drug testing. The Department of Transportation requires specific procedures, documentation standards, and certification requirements that go beyond what many labs handle in their routine testing operations. When you process DOT tests, you’re not just running samples through your equipment—you’re part of a federal compliance system that directly impacts transportation safety across the country.
The scope of DOT testing covers employees in safety-sensitive transportation positions. This includes commercial truck drivers, bus drivers, railroad workers, maritime employees, pipeline workers, and aviation personnel. SAMHSA outlines DOT drug testing as a federally mandated protocol targeting these specific transportation workers to ensure they remain fit for duty. As a laboratory manager, you need to recognize that DOT employers must follow strict testing protocols at specific points in employment: pre-employment, post-accident, random, reasonable suspicion, and return-to-duty testing. Each of these testing scenarios has unique documentation and chain-of-custody requirements that differ from non-DOT testing. Your lab’s procedures must accommodate these variations, and your staff needs training on how DOT tests differ from regular workplace screening.
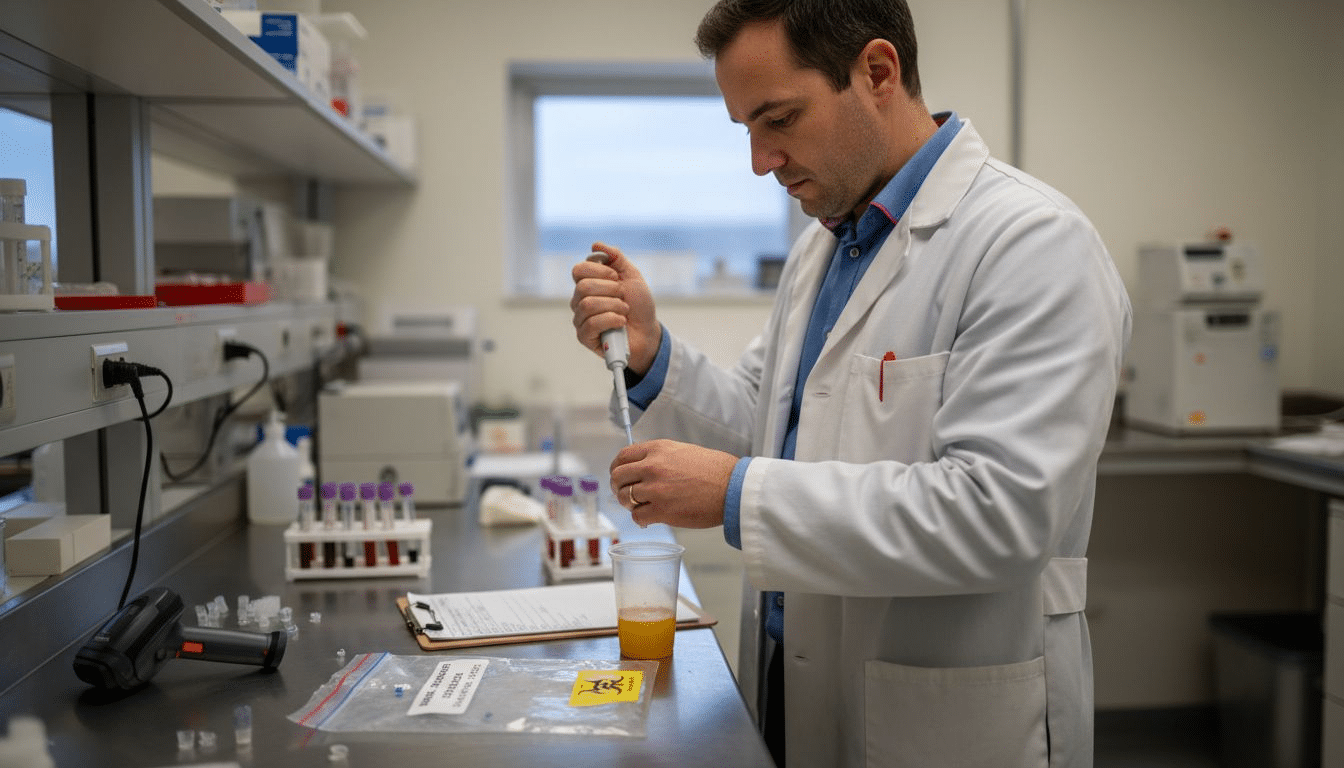
What makes DOT testing unique in your lab is the mandatory involvement of qualified personnel at every stage. The collection process requires a SAMHSA-certified Collector, the laboratory analysis must be performed by a SAMHSA-certified facility with certified analysts, and the results must be reviewed by a Medical Review Officer (MRO) before being reported to the employer. The framework for federally regulated drug testing includes roles such as Substance Abuse Professionals who evaluate employees who test positive and ensure they receive appropriate intervention before returning to safety-sensitive duties. Your laboratory sits at the critical middle point of this process. You receive specimens that must be handled with specific chain-of-custody documentation, you analyze them using DOT-approved methodologies, and you report results in exact compliance with federal guidelines. Any deviation from these procedures can invalidate a test result and expose both your lab and the employer to liability.
The testing panels themselves follow a standardized format in DOT programs. The five-panel test screens for marijuana, cocaine, opioids, amphetamines, and phencyclidine (PCP). However, some employers expand to a ten-panel test that adds additional opioids, benzodiazepines, barbiturates, and other substances. The distinction between different drug test panel options matters because DOT regulations specify which panels are acceptable for different transportation modes. Your lab must verify with each employer which panel they require and ensure your testing capability matches their DOT-mandated needs. Initial screening uses immunoassay methods, and any positive result requires confirmatory testing using gas chromatography-mass spectrometry (GC-MS) before it can be reported as a confirmed positive.
Compliance in DOT testing centers on three non-negotiable elements: accuracy, documentation, and timing. Your lab must maintain SAMHSA certification, keep detailed records of all test results and chain-of-custody procedures, and meet strict reporting timelines. When a specimen arrives at your facility, you become responsible for maintaining its integrity and ensuring the test results meet federal standards. Laboratory managers often find that implementing DOT-compliant procedures requires additional training for staff, more rigorous documentation systems, and sometimes upgraded equipment to meet certification requirements. The investment pays off because DOT testing typically commands higher fees than standard workplace testing, reflecting the additional complexity and regulatory burden your lab assumes.
Here’s how DOT and non-DOT laboratory drug testing procedures compare:
| Aspect | DOT Drug Testing | Non-DOT Drug Testing |
|---|---|---|
| Regulatory Oversight | Federally mandated under 49 CFR Part 40 | Guided by private/employer policies |
| Required Certification | SAMHSA laboratory and collector certification | Varies; often none required |
| Test Panel Standardization | Fixed 5-panel (marijuana, cocaine, opiates, PCP, amphetamines) | Flexible; panels vary by employer |
| Confirmation Requirement | Mandatory GC-MS confirmation for positives | Often at employer discretion |
| Documentation Level | Extensive chain-of-custody, MRO review required | Varies; may be less rigorous |
| Reporting Process | Results sent to MRO, not employer directly | Results often reported to employer |
Pro tip: Before accepting DOT testing samples, verify that your laboratory holds current SAMHSA certification for the specific substances you’ll be testing and maintain detailed training records for all personnel involved in collection and analysis—these certifications and records form the foundation of your DOT compliance defense if ever questioned by auditors or in legal proceedings.
DOT Drug Test Types and Testing Methods
Unlike non-DOT workplace testing where employers can choose from various panel sizes and substances, DOT regulations lock you into a specific, standardized approach. The federal requirement mandates a 5-panel urine test that screens for five specific substances: marijuana, cocaine, opiates, phencyclidine (PCP), and amphetamines/methamphetamines. This consistency across all DOT-regulated employers means your laboratory doesn’t need to maintain multiple test configurations for different DOT clients—everyone uses the same five-panel format. However, some DOT employers add a sixth substance to their testing program: MDMA (ecstasy). When this happens, the test becomes a 6-panel, but the core five substances remain mandatory. The standardized nature of DOT drug testing involving a fixed 5-panel urine test exists precisely because federal regulators want consistency in how transportation safety is monitored nationwide.
The testing methodology your lab uses must follow a two-stage process that the Department of Transportation requires without exception. Stage one begins with initial screening, typically using immunoassay technology that detects the presence of drug metabolites in the urine specimen. Your lab runs the sample through an automated analyzer or performs the test using immunoassay reagents, which gives you a fast preliminary result. If the initial screening comes back negative, that result goes directly to the Medical Review Officer for reporting. But if it comes back positive for any of the five substances, you cannot report it as a confirmed positive yet. You must move immediately to stage two: confirmatory testing. The gold standard confirmatory method uses gas chromatography-mass spectrometry (GC-MS) to detect specific drug compounds, which provides definitive identification and quantification of the drug present. This two-step process eliminates false positives and gives you the scientific credibility that federal regulations demand. The GC-MS confirmatory testing is where many labs encounter equipment investment requirements, since the analyzer itself represents significant capital expenditure, but it’s non-negotiable for any laboratory processing DOT tests.
Your lab must understand the critical distinction between detection cutoff levels for initial screening versus confirmatory testing. DOT regulations specify different threshold concentrations for each stage. For example, the initial screening cutoff for marijuana metabolites is 50 nanograms per milliliter (ng/mL), but the confirmatory GC-MS cutoff is 15 ng/mL—meaning a specimen can pass initial screening but still test positive on confirmatory testing if the actual concentration falls between these two thresholds. This matters because it directly impacts your lab’s quality control procedures and your ability to troubleshoot unexpected results. Your technical staff must understand why a specimen might show negative on the screening but positive on confirmation, which sounds counterintuitive but reflects the sensitivity differences between the two methodologies. Similarly, opiates have a 300 ng/mL screening cutoff but a 300 ng/mL confirmatory cutoff, while cocaine metabolites use 300 ng/mL for both stages. The amphetamine screening cutoff of 500 ng/mL drops to 250 ng/mL for confirmatory testing. These specific values aren’t just numbers on a regulatory page—they define what your equipment must detect and what your procedures must accommodate.
Summary of required detection cutoff levels for DOT drug test panels:
| Substance | Initial Screening Cutoff (ng/mL) | Confirmatory Cutoff (ng/mL) |
|---|---|---|
| Marijuana (THC) | 50 | 15 |
| Cocaine | 300 | 300 |
| Opiates | 300 | 300 |
| Amphetamines | 500 | 250 |
| PCP | 25 | 25 |
Note: Lower confirmatory cutoffs increase test sensitivity and accuracy.
The practical workflow in your lab for each DOT specimen follows this sequence: receive the sample with complete chain-of-custody documentation, verify specimen integrity and proper labeling, perform the initial immunoassay screening on all specimens, separate negative from presumptively positive results, conduct GC-MS confirmatory testing on all presumptively positive specimens, and prepare results for review by a Medical Review Officer before reporting to the employer. The confirmatory testing step creates a natural bottleneck in your workflow because GC-MS analysis takes longer than immunoassay screening—typically several hours compared to minutes for initial screening. This timing difference means you need to batch your confirmatory tests efficiently and manage your queue strategically. Your lab’s turnaround time commitments to clients should account for this two-stage process, recognizing that you cannot rush the confirmatory stage without compromising result reliability. Some laboratories use rapid GC-MS systems to accelerate this phase, but the testing rigor remains identical regardless of equipment speed.
Pro tip: Implement a clear sample tracking system that flags presumptively positive specimens immediately after initial screening so your staff knows which samples require GC-MS confirmation before handling the next batch—this prevents accidental reporting of unconfirmed results and maintains the workflow efficiency your lab needs to meet client timelines.
Key Regulations and 2026 Testing Updates
The regulatory foundation for DOT drug testing rests on two major pieces of federal legislation: the Omnibus Transportation Employee Testing Act of 1991 and 49 CFR Part 40, which provides the detailed procedural framework that governs every aspect of how your laboratory must operate. These regulations aren’t suggestions or guidelines—they’re mandatory requirements backed by federal enforcement authority. The specific testing triggers mandated by law include pre-employment testing before an employee starts work in a safety-sensitive position, random testing conducted throughout employment, post-accident testing following certain transportation incidents, and reasonable suspicion testing when an employer has specific articulable facts suggesting substance use. Return-to-duty testing is also required for employees who previously tested positive and have completed required interventions. Understanding these testing scenarios matters for your lab because each one carries slightly different procedural requirements and documentation standards. DOT drug testing regulations under 49 CFR Part 40 outline these testing triggers and enforcement requirements that directly impact how your lab receives, processes, and reports specimens.
What’s changing in 2026 should be on your strategic planning radar right now. The Department of Transportation and SAMHSA have been working on mandatory guideline updates that will refine testing protocols, enhance data security measures, and strengthen enforcement mechanisms to address evolving drug use trends. One significant change involves expanding the scope of specimen validity testing, which checks for adulterants and dilution attempts that employees sometimes use to mask drug use. Currently, your lab may perform validity testing, but 2026 updates are expected to make more comprehensive adulteration detection mandatory for all DOT tests. This means you may need to invest in additional testing capabilities or partner with laboratories that can perform expanded adulterant panels. Another anticipated update involves new procedures for specimen handling and enhanced confidentiality protections that strengthen data security throughout the testing chain. These changes reflect technological advancements and lessons learned from recent compliance audits across the transportation industry. Your lab should begin reviewing current procedures now to identify gaps that the 2026 updates will address, giving you time to implement changes before they become mandatory.
The practical implication of these regulatory frameworks is that your laboratory must maintain current knowledge of 49 CFR Part 40 and stay informed about announced regulatory changes. Many labs miss critical updates by assuming their current procedures will remain acceptable indefinitely. The reality is that DOT regulations evolve, and your lab’s compliance status is judged against the current version of the regulations at any given time. This creates an ongoing requirement to monitor federal registers, attend industry conferences, and maintain relationships with compliance consultants who track regulatory changes. The 2026 updates will likely introduce new equipment requirements, revised specimen collection procedures, and potentially expanded drug panels that some DOT employers will adopt. While the core five-panel test will almost certainly remain the federal minimum, certain employers may be permitted or required to add additional substances like synthetic cannabinoids or fentanyl to their testing protocols. Your lab needs to be positioned to offer expanded panels as soon as regulatory permission is granted, which means equipment upgrades and staff training should begin before the official 2026 implementation date. Additionally, the reinforced confidentiality protections expected in 2026 may require system upgrades to how you store and transmit test results electronically, potentially involving enhanced encryption or new software platforms.
Your laboratory’s compliance posture must account for both current regulations and anticipated changes. This means establishing a regulatory monitoring process, documenting your current procedures against existing CFR requirements, and creating a timeline for implementing anticipated 2026 changes. Many labs find it cost-effective to conduct a compliance assessment now with external auditors who understand the incoming regulatory landscape, identifying any current gaps before they create audit findings. The DOT takes compliance seriously, and penalties for violations range from warning letters to significant fines and potential loss of certification. Labs that proactively address regulatory updates demonstrate good faith compliance efforts that regulators view favorably. Your documentation showing that you began implementing 2026 requirements before the mandate date protects your lab in audit situations. The regulatory environment is moving toward stricter controls and enhanced accountability, which aligns with the overall goal of improving transportation safety through more reliable substance screening.
Pro tip: Schedule a meeting with a DOT compliance consultant in the next quarter to review your current procedures against 49 CFR Part 40 and discuss anticipated 2026 changes—doing this before regulatory deadlines arrive gives you months to budget for equipment upgrades and staff training rather than scrambling for last-minute compliance solutions.
Employer Roles and Laboratory Compliance Duties
DOT drug testing success depends on a clear division of responsibilities between employers and laboratories, each with specific, non-negotiable duties. Your laboratory doesn’t operate in isolation—you’re one critical component of a larger compliance ecosystem where employers initiate testing, your lab analyzes specimens, and Medical Review Officers (MROs) interpret results. Understanding this partnership structure helps you recognize what falls within your lab’s control and what depends on employers maintaining their end of the bargain. Employers must select only SAMHSA-certified laboratories for DOT testing, which means your certification status directly affects whether employers can legally use your services. But certification alone isn’t enough. Employers have specific roles including ensuring employees in safety-sensitive positions undergo required testing and maintaining proper documentation while coordinating with certified laboratories like yours. Your lab benefits when employers understand their responsibilities because it reduces specimen handling errors, ensures proper chain-of-custody documentation, and creates clear communication channels when results need clarification.
Your laboratory’s compliance duties extend across every phase of the testing process, starting the moment a specimen arrives at your facility. You must verify that the specimen was collected by a SAMHSA-certified Collector using proper procedures, document the complete chain-of-custody without breaks or gaps, and store the specimen under appropriate conditions pending analysis. The actual testing phase requires you to perform initial screening using approved methodologies and conduct confirmatory GC-MS testing on all presumptively positive results. But your responsibilities don’t end when the analysis is complete. You must generate a detailed laboratory report that includes specific information: the drug or metabolite identified, the quantity detected, the method used, the date of testing, and your laboratory’s certification number. This report goes to the Medical Review Officer, not directly to the employer, which creates a built-in quality control step. Your laboratory must also maintain strict quality assurance standards and adhere to defined testing procedures to ensure valid results with proper chain of custody and confidentiality, which means your documentation systems must be ironclad. Any gap in your record-keeping can invalidate an otherwise legitimate test result and expose your lab to liability.
The relationship between employers and your laboratory requires clear communication about timelines and procedures. Employers operate under pressure to get results quickly so they can make employment decisions, but your lab cannot sacrifice accuracy for speed. This is where written service agreements become critical. Your agreements with DOT employers should specify your standard turnaround time for initial screening results, your timeline for confirmatory testing, and what constitutes an urgent or expedited request. The agreement should also clarify who pays for testing, whether employers can request additional testing beyond the mandated five-panel test, and how you handle specimen integrity issues like dilution or adulteration. Many labs find that employers don’t fully understand the two-stage testing process and expect confirmed results within hours of specimen collection. Setting realistic expectations upfront prevents disputes later. Additionally, your lab must establish procedures for handling requests from employers about results. You never discuss results directly with employers—that’s the MRO’s role—but you do provide technical information if the MRO needs clarification about your methodology or findings. This three-party structure exists to protect employee privacy while ensuring employers get accurate information for employment decisions.
Compliance also means understanding what happens after your lab reports results. Employers must designate someone to receive test results from the MRO and manage the return-to-duty process if an employee tests positive. Your lab’s responsibility at this point involves maintaining records and being prepared to provide information if the result is challenged legally. This is where your documentation becomes invaluable. If an employee contests their positive result months later through legal action, your complete chain-of-custody records, equipment maintenance logs, analyst certifications, and quality control documentation either support the validity of the result or reveal problems that could undermine it. Many litigation cases hinge on whether the laboratory maintained adequate records, not on whether the test was performed correctly. Your lab’s compliance culture should treat documentation as equally important as analytical accuracy. This means training staff to understand that writing down information in real-time is part of testing, not a separate administrative task. When a technician logs a specimen, notes the exact time of receipt, records equipment lot numbers, and documents quality control results, they’re building the foundation for a defensible test result that will hold up under scrutiny.
Pro tip: Create a compliance checklist that your lab team reviews before reporting any DOT test result, verifying that the specimen arrived with proper chain-of-custody documentation, that both screening and confirmation were performed, that all results are documented with dates and times, and that your SAMHSA certification number appears on the report—this simple discipline prevents oversights that could invalidate an otherwise legitimate result.
Risks, Penalties, and Avoiding Common Mistakes
Non-compliance with DOT drug testing regulations carries consequences that extend far beyond corrective action notices. Your laboratory faces direct penalties if audits reveal violations, including fines that can accumulate quickly, loss of SAMHSA certification that eliminates your ability to process DOT tests, and potential litigation from employers or employees who claim damages from improper testing. The financial impact varies based on violation severity, but even a single instance of improper chain-of-custody documentation or failure to conduct confirmatory testing can trigger regulatory action. Beyond the immediate financial penalties, your lab’s reputation becomes a liability. Word travels fast in transportation and logistics industries about laboratories that cut corners or produce questionable results. One compliance failure can cost you multiple employer clients who shift their testing to laboratories with spotless compliance records. The stakes are particularly high because transportation safety directly affects public welfare—regulators take DOT testing violations seriously as matters of public interest, not merely administrative infractions. Failing to maintain strict compliance with DOT drug testing protocols risks fines, loss of licenses, and litigation that can severely damage both your lab’s operations and financial position.
Common mistakes that laboratory managers encounter reveal patterns worth learning from without having to experience them firsthand. The most frequent error involves chain-of-custody documentation gaps, where specimens aren’t properly logged at receipt, transfer steps aren’t documented, or custody breaks occur without explicit notation. These gaps don’t necessarily indicate wrongdoing, but they create legal vulnerabilities because missing documentation makes it impossible to defend the integrity of a test result. Another common mistake is rushing confirmatory testing timelines. Laboratories sometimes compress GC-MS analysis schedules to meet employer expectations for quick results, inadvertently skipping quality control steps or combining samples in ways that violate protocol. The pressure to deliver results quickly is real, but sacrificing analytical rigor defeats the entire purpose of the two-stage testing process. A third frequent error involves incomplete analyst training. Your staff might understand how to operate equipment but not fully grasp the regulatory reasoning behind specific procedures, which leads to shortcuts when facing unexpected specimen issues. When a specimen appears diluted or shows unusual characteristics, an inadequately trained technician might make judgment calls that violate protocol rather than documenting the issue and seeking guidance. Common mistakes such as delays in testing or improper specimen handling risk non-compliance and create legal exposure that affects both your lab and the employers relying on your results.
Specimen handling errors represent a particularly insidious category of mistakes because they can occur with good intentions but produce invalid results. Improper storage temperature before analysis can degrade metabolites and produce false negatives. Using contaminated collection containers or glassware introduces adulterants that create false positives. Mixing specimens or mislabeling during analysis makes it impossible to determine which result belongs to which employee. These errors often go undetected until months later when an employee contests a result and your records reveal the handling mistake. At that point, your lab bears the burden of proof that the error didn’t affect the result, a position that’s difficult to defend. Another category involves documentation errors that seem minor but carry significant consequences. Failing to record the exact time of specimen receipt makes it impossible to verify that samples were analyzed within required timeframes. Not documenting equipment maintenance schedules raises questions about whether the analyzer was functioning properly when the test was performed. Omitting the lot number of reagents used prevents verification that you didn’t use expired or defective testing materials. Each of these documentation failures individually might seem minor, but collectively they undermine the defensibility of your entire testing process.
Preventing mistakes requires building compliance into your lab’s culture and systems rather than treating compliance as an administrative burden separate from testing operations. Implement written standard operating procedures (SOPs) that specify exactly how each task must be performed, from specimen receipt through result reporting. Train all staff annually on these procedures and maintain documentation proving that training occurred, which demonstrates your commitment to compliance if ever audited. Create redundant verification steps where a second person independently checks critical information before specimens move to the next testing phase. Establish an internal audit schedule where someone with authority reviews chain-of-custody documentation, quality control results, and analyst qualifications on a regular basis, identifying potential problems before regulators discover them. Use equipment that provides automated documentation of analysis parameters, reducing human error in recording test conditions. Require your quality assurance manager to sign off on all DOT test reports before they go to Medical Review Officers, creating a final compliance checkpoint. Most importantly, communicate to your staff that compliance failures aren’t tolerated and that cutting corners creates liability for everyone working in the lab. When staff understand that compliance protections their jobs and the lab’s viability, they approach procedures with appropriate seriousness. The most successful laboratories treat DOT compliance as inseparable from their identity, not as something they’re forced to do.
Pro tip: Conduct a self-audit every quarter where you randomly select 10 completed DOT test cases and verify that chain-of-custody documentation is complete, both screening and confirmation were performed, results are documented with exact times and dates, equipment maintenance records exist for the analysis dates, and analyst qualifications were current—this proactive review catches gaps before regulators do and demonstrates compliance commitment if your lab is ever audited.
Strengthen Your DOT Drug Testing Compliance with Trusted Supplies
Compliance with DOT drug testing regulations demands precision, detailed documentation, and reliable testing methods that protect your laboratory from costly penalties and reputational damage. The challenges of maintaining SAMHSA certification, performing accurate GC-MS confirmatory tests, and meeting evolving 49 CFR Part 40 requirements leave little room for error. Your lab needs high-quality, FDA-approved drug test cups and specimen collection supplies to ensure every step—from initial screening to chain-of-custody—meets federal standards.
Visit RapidTestCup to explore our extensive catalog of compliant, CLIA-waived drug testing kits and collection accessories designed specifically for professional use. We offer fast shipping, bulk discounts, and trusted products that empower laboratories, clinics, and safety-focused employers to uphold the highest DOT drug testing standards. Don’t risk non-compliance or delays—equip your team today with supplies from RapidTestCup and stay ahead of the 2026 regulatory updates to safeguard your lab’s reputation and integrity.
Frequently Asked Questions
What is DOT drug testing?
DOT drug testing is a federally mandated substance screening program aimed at ensuring safety in transportation-related jobs. It involves a specific regulatory framework established under the Omnibus Transportation Employee Testing Act of 1991, focusing on employees in safety-sensitive positions.
Why is compliance important in DOT drug testing?
Compliance is crucial in DOT drug testing because failure to adhere to federal regulations can result in serious penalties, including fines and loss of certification for laboratories. Maintaining compliance ensures the integrity of the testing process and upholds safety in the transportation industry.
What are the different types of DOT drug tests?
DOT drug testing typically includes five main types: pre-employment, random, post-accident, reasonable suspicion, and return-to-duty testing. Each type has unique documentation and procedural requirements that laboratories must follow to remain compliant.
How does the testing methodology differ from non-DOT drug testing?
DOT drug testing follows a two-stage process involving an initial screening test using immunoassays followed by confirmatory testing with gas chromatography-mass spectrometry (GC-MS) for positive results. This rigorous process ensures higher accuracy compared to many non-DOT drug tests, which may not always require confirmatory testing.




